- Actinic Keratosis
- Basal Cell Carcinoma
- Squamous Cell Carcinoma
- Melanoma
- Kaposi's Sarcoma
- Anogenital Carcinoma
Actinic Keratosis
- Rough, red or pink scaly patches on sun-exposed areas of the skin,usually <0.5cm in diameter
- Precurser lesion for squamous cell carcinoma
- Up to 1% of these lesions can develop into a Squamous Cell Carcinoma
An early warning sign of skin cancer is the development of an actinic keratosis. Actinic keratoses are precancerous skin lesions that result from chronic sun exposure. They are typically < 0.5cm in diameter, pink or red in color and rough or scaly to the touch. They occur on sun-exposed areas of the skin (face, scalp, ears, backs of hands or forearms). Actinic keratoses may start as small, red, flat spots but grow larger and become scaly or thick, if untreated. Sometimes they are easier to feel than to see. There may be multiple lesions next to each other.
Early treatment of actinic keratoses may prevent their change to cancer. These precancerous lesions affect more than 10 million Americans. People with one actinic keratosis usually develop more. Up to 1% of these lesions can develop into a squamous cell cancer.
Actinic keratoses are most common in people older than 40, but can also appear in younger individuals with extensive sun exposure. Because they can turn cancerous affected areas should be regularly examined and treated by a primary care physician or dermatologist.


Basal Cell Carcinoma
- Raised, pink, waxy bumps that may bleed following minor injury
- May have superficial blood vessels and a central depression
- Locally invasive
- Rarely metastasizes
- Organ transplant recipients have a 10-fold higher risk for Basal Cell Carcinoma compared to the general population (5)
Basal cell carcinoma is the most common type of non-melanoma skin cancer. This type of cancer often looks like a pink waxy bump that may bleed following minor injury. There may be irregular blood vessels on its surface and its center may be sunken in. Large basal cell carcinomas may have oozing or crusted areas.
Basal cell carcinomas typically occur on sun-exposed skin of the face, ears, neck and trunk but may also occur on the arms or legs. Basal cell carcinomas grow slowly and rarely spread to other parts of the body (metastasize). However, if left untreated, they can become locally invasive and destroy surrounding muscle, bone and nerves causing significant disfigurement and functional problems.
There are several subtypes of basal cell carcinoma. Some are more aggressive than others. The subtype of basal cell carcinoma is identified by skin biopsy and examination under a microscope.
What causes basal cell carcinoma? The most common cause of basal cell carcinoma is ultraviolet light (UV), specifically ultraviolet B (UVB, 290-320 nm). Indoor tanning, fair-skinned complexion, prior radiation exposure and inherited genetic conditions such as nevoid basal cell carcinoma syndrome or Basex's syndrome are other important risks factors.
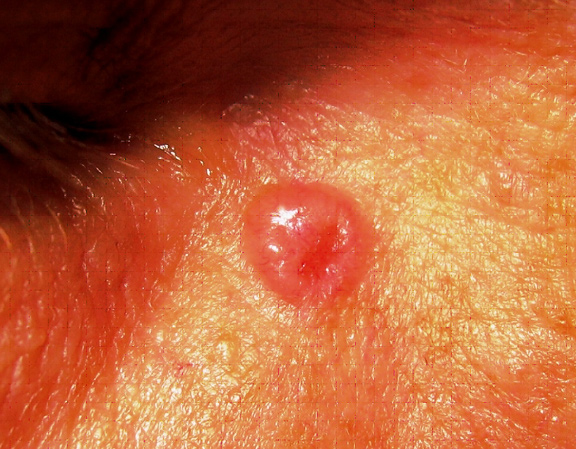
Translucent pearly pink papule near the right eye.

This tumor has the characteristic translucent, pearly quality with superficial blood vessels. Notice its depressed, almost scar-like appearance, commonly seen in the infiltrative subtype of basal cell carcinomas.
Squamous Cell Carcinoma
- Dull red, rough, scaly raised skin lesions
- Occur most frequently on sun exposed areas (head, neck, ears, lips, back of the hands and forearms)
- Sites particularly associated with elevated risk for recurrence or metastasis include: ear, lip/perioral, nose, periorbital, genitalia
- Most common skin cancer that occurs in pediatric and adult transplant recipients
- Squamous Cell Carcinoma tumors can grow very rapidly
- Mutiple cancers can occur simultaneously
- Squamous Cell Carcinoma tends to be more invasive and more aggressive in transplant patients
- Organ transplant recipients have a 65-fold higher risk for Squamous Cell Carcinoma and 20-fold higher risk for Squamous Cell Carcinoma of the lip compared to the general population (6)
- Adult transplant patients tend to develop Squamous Cell Carcinoma 5-7 years following transplant
- Pediatric transplant patients (patients who received their transplants before the age of 18) tend to develop Squamous Cell Carcinoma an average of 10 years following transplant (7)
- Pediatric transplant patient have higher risk for Squamous Cell Carcinoma of the lip compared to adult transplant patients
- Local recurrance rate ~13% in adult transplant patients (8, 9)
- Metastatic rate ~2% in general population
Squamous cell carcinoma is the second most common skin cancer after basal cell carcinoma. Squamous cell carcinomas are often described as enlarging red bumps, sometimes with a rough, scaly, or crusted surface. They may also look like flat reddish patches in the skin that grow slowly. If untreated, they can become ulcerated (open sores). Most squamous cell carcinomas grow slowly. Occasionally, they may occur quite rapidly, particularly in patients who are immunosuppressed.
Squamous cell carcinomas occur most frequently on sun-exposed areas such as the head, neck, ears, lips, back of the hands and forearms.
This cancer rarely metastasizes (spreads to lymph nodes or other organs), although distant spread happens more frequently than in basal cell carcinoma. The squamous cell carcinoma that has metastasized typically is:
- greater than 2cm in diameter or greater than 4mm in depth
- in a site previously exposed to radiation
- in a patient with a history of solid-organ transplantation
When squamous cell carcinoma does metastasize, it most commonly travels to the local lymph nodes.
Squamous cell carcinoma is the most common skin cancer in organ transplant recipients.




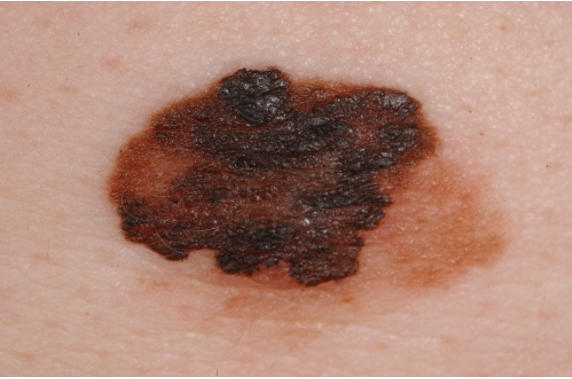
Melanoma
- Neoplasm of pigment (melanin) producing cells
- Brown or black skin lesion with irregularities in symmetry, border and coloration
- Prognosis dependent on depth of invasion
~100,000 new cases of melanoma are diagnosed in the United States each year- Only 4% of diagnosed skin cancer, but 77% of skin cancer related deaths
- Organ transplant recipients have a 3 to 4-fold higher risk for melanoma compared to general population (1)
- Melanoma accounts for ~6% of post transplant skin cancers in adult transplant recipients (7)
- Melanoma accounts for 12-15% of post transplant skin cancers in pediatric organ transplant recipients (7)
- Transplant recipients with a pre-transplant history of melanoma have a high risk of recurrence (~20%) (11)
Melanoma is the most dangerous type of skin cancer. Although melanoma makes up only 4% of skin cancers, it causes 77% of skin cancer deaths. About 100,000 cases of melanoma are diagnosed each year.
Melanoma typically presents as a brown or black spot with irregularities in symmetry, border and color. Melanoma may develop within an existing mole or on previously normal appearing skin. Melanoma has a high fatality rate because its cells can break off and spread throughout the body (metastasize).
When melanoma is caught early, your chances for successful treatment are much higher.
The ABCDEs of Melanoma
These characteristics are used by dermatologists to classify melanomas. Look for these signs: Asymmetry, irregular Borders, more than one or uneven distribution of Color, or a large (greater than 6mm) Diameter. Finally, pay attention to the Evolution of your moles - know what's normal for your skin and check it regularly for changes.
If you see one or more of these, make an appointment with a dermatologist immediately. Please note that not all melanomas fall within the ABCDE parameters so visit your dermatologist regularly to catch any potiential issues early.
 |
A - Asymmetrical ShapeMelanoma lesions are often irregular, or not symmetrical, in shape. Benign moles are usually symmetrical. |
 |
B - BorderTypically, non-cancerous moles have smooth, even borders. Melanoma lesions usually have irregular borders that are difficult to define. |
 |
C - ColorThe presence of more than one color (blue, black, brown, tan, etc.) or the uneven distribution of color can sometimes be a warning sign of melanoma. Benign moles are usually a single shade of brown or tan. |
 |
D - DiameterMelanoma lesions are often greater than 6 millimeters in diameter (approximately the size of a pencil eraser). |
E - Evolution
The evolution of your mole(s) has become the most important factor to consider when it comes to diagnosing a melanoma. Knowing what is normal for YOU could save your life. If a mole has gone through recent changes in color and/or size, bring it to the attention of a dermatologist immediately.

This 38 year old patient noticed that a previously flat mole had changed and become larger in diameter and protruded outward from his skin (This fulfills the E for Evolution rule of the ABCDE’s).

Melanoma can occur in unusual areas, including the hands, feet and even the eye
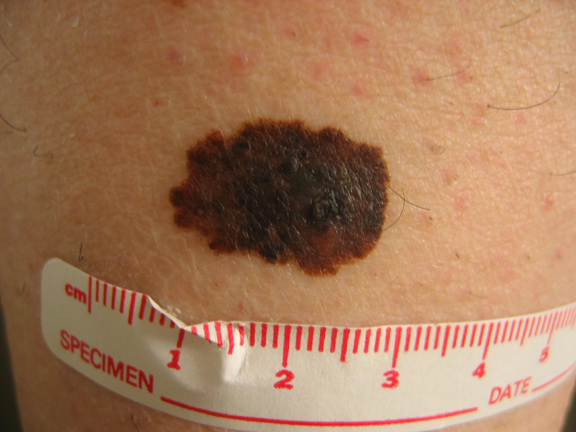
This melanoma is asymmetric, has an irregular border, has multiple colors within the lesion (brown, black, tan) and is > 0.6cm in diameter.
Kaposi's Sarcoma
- Rare, cancer of the cells that line blood vessels (endothelial cells)
- Clinically: brownish-red to blue colored skin lesions found most frequently on legs and feet
- Caused by Human Herpes Virus 8 (HHV-8) which causes the cells that line blood vessels (endothelial cells) to become cancerous in the setting of profound and prolonged immunosuppression
- Typically occurs in patients of Middle Eastern, Jewish, Mediterranean or African descent where HHV-8 in endemic
- Two main forms of Kaposi's Sarcoma exist
- Cutaneous/Mucocutaneous
- Visceral
- Most common form that occurs in pediatric transplant patients (7)
- Most pediatric cases occur while the patient is < 18 years old
- Kaposi's Sarcoma tumors can affect the gastrointestinal system, lymph nodes and lungs
- The visceral form is considered more serious than the cutaneous/mucocutaneous form

Anogenital Carcinoma
- These include tumors of the vulva, scrotum, penis, perianal skin and anus
- Occur at 30-100 fold higher incidence in transplant patients than the general population
- Most common in females
- Ratio of female to male patients 2 to 1 (adult transplant patients)
- Ratio of female to male patients 8.5 to 1 (pediatric transplant patients)
- Tend to occur ~12 yrs after transplantation (mean age of 27y/o) in pediatric transplant patients and ~7yrs after transplant in adult transplant recipients
- Clinically:
- Tend to be multiple, extensive, or both
- May resemble wart-like lesions
- Risk factors include:
- Mutiple sexual partners, HPV infection, hx of herpes genitalis, heavy smoking, high level of immunosuppression
- Post-adolescent female transplant recipients should have regular gynecologic examination of the anogenital region



